Team Uncovers New Regulators with Shorter Path to Clinical Use
Cardiovascular diseases are the leading cause of death in the U.S. With one in every four deaths occurring each year, the five-year survival rate after a heart attack is worse than most cancers. A big part of the problem is the inability of the human heart to effectively repair itself after injury. A team of University of Houston researchers is trying to change that.
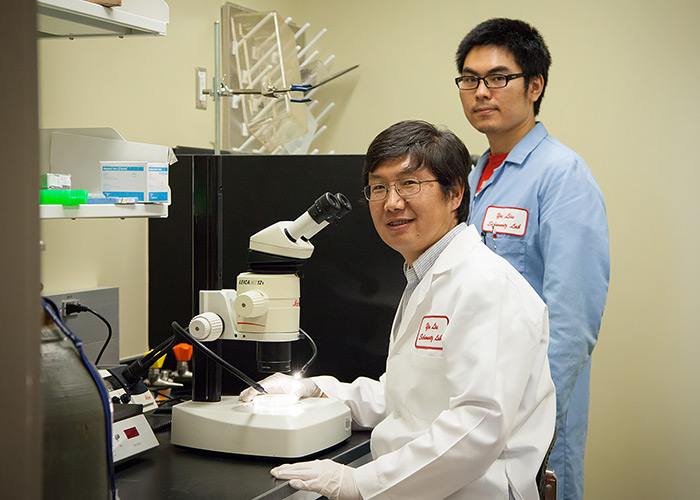
University of Houston developmental biologists Yu Liu and Xiaopeng Shen examine stem
cells in Liu’s lab.Physicians and biologists are developing strategies to help regenerate heart muscle
cell formation. Among them are developmental biologists in UH’s College of Natural
Sciences and Mathematics, whose work has added novel, powerful tools to achieve this.
Their findings were published in the Aug. 10 early edition of the Proceedings of the National Academy of Sciences, one of the world’s most-cited multidisciplinary scientific journals.
The human heart is an organ that doesn’t regenerate, and the number of heart muscle cells drops as a person ages. Cells lost during injuries, such as from a heart attack, are gradually replaced by connective tissue, a process called fibrosis. This leads to the loss of pump function, which is the underlying reason cardiovascular diseases are as deadly as cancers.
“We have uncovered new regulators of heart formation,” said assistant professor of biochemistry Yu Liu, one of the lead authors of the study. “Compared to most others, these new regulators, which are a small RNA species called microRNAs, act early in the multistep heart formation process. They are easier to deliver into human bodies, and thus have a shorter path to clinical use.”
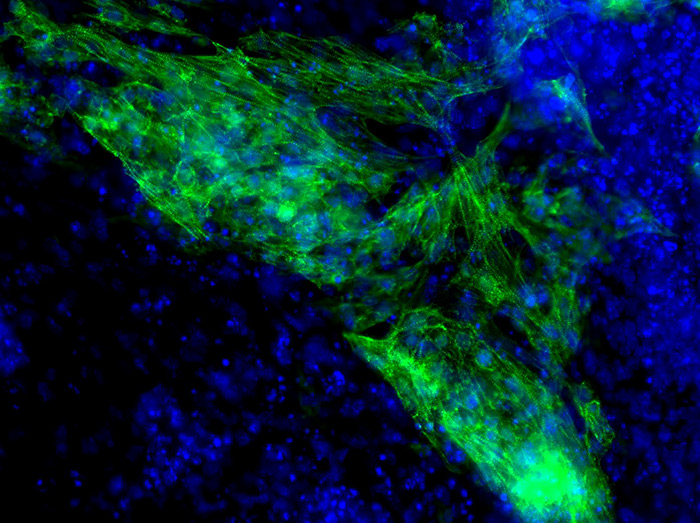
In trying to find a solution, Liu and his colleagues focused on learning how a heart is formed in an embryo. Specifically, they are curious as to whether the new regulators they uncovered will convert an abundant cell type, called human fibroblasts, into heart muscles. Robert Schwartz, Cullen Distinguished Professor of biochemistry and also an author on this study, is a pioneer in making heart muscle cells from fibroblasts, which is now a widely adopted strategy.
A team of developmental biologists at the University of Houston have uncovered new
regulators of heart formation that are easier to deliver into human bodies, and thus
have a shorter path to clinical use.“We were the first in converting human fibroblasts into cardiomyocytes,” Schwartz
said. “I expect these microRNA regulators to be potent, either acting alone or in
combination with the existing agents we have.”
In a project with NASA’s Center for the Advancement of Science in Space, Schwartz is exploring how the unique environment in space can assist in the creation of heart muscle cells out of fibroblasts. The microRNAs they uncovered will add substantially to his toolbox in this effort.
Once considered genetic junk, microRNAs have emerged as a major player in gene regulation. Using mouse genetic tools, Liu and his team were able to track the process of heart muscle cell formation in a dish. Their work involved several screening steps. Most importantly, they first identified approximately 140 microRNAs in the earliest ancestor cells of the heart. Next, they screened for the ones that function in driving heart muscle cell formation, and the miR-322/503 cluster emerged as the top finding in both screenings and laid the basis for their work.
Supported by multiple grants from the American Heart Association, Liu hopes to be able to use these microRNAs to treat human heart attack and subsequent heart failure within the next five to 10 years. Beyond this manuscript, they have developed several mouse models in house and hope to make more exciting discoveries down the road.
Additional UH collaborators on this study included Preethi Gunaratne, associate professor of biochemistry and a genome sequencing pioneer in the field of microRNA research, and Xiaopeng Shen, a postdoctoral fellow in Liu’s lab and first author of the article. Part of the research included in the paper is Shen’s thesis work, which he completed as a graduate student in biochemistry at UH.
- Lisa Merkl, University Media Relations